MEET THE SURGEON

Dr Raymond K. Wurapa, MD
Orthopedic Surgeon
Orthopedic ONE, Columbus Ohio
Specialist in hand, wrist and upper extremity surgery
Fellow of Philadelphia Hand To Shoulder Center/
Thomas Jefferson University
Philadelphia Pennsylvania
OVERVIEW
A 25-year-old right-hand-dominant female presented to Dr Wurapa three days after being involved
in a motor vehicle accident.
X-rays showed unstable fracture patterns involving the third and fourth metacarpal shafts. Given her young age, dominant hand involvement and fracture patterns; reduction and fixation was recommended and achieved with the NX Nail.
CASE INTRODUCTION
A 25-year-old right-hand-dominant female customer service associate presented with a tender and swollen right hand, three days after a motor vehicle accident. The patient was referred through the Emergency Department as x-rays revealed she had sustained multiple fractures to her third and fourth metacarpals.
CASE PRESENTATION
Referred from the Emergency Department the patient presented to Dr Wurapa three days after the accident. At this time, she had significant pain that was not resolving and concern about increased difficulty performing daily tasks. Review of her x-rays showed both fractures to be extra-articular, with a non-displaced long oblique fracture of the third metacarpal and a displaced long oblique
fracture of the fourth metacarpal.
Below: Pre-Operative Imaging

PRE-OPERATIVE PLAN
Given the patient’s young age, dominant hand involvement and morbidity, reduction and fixation was recommended. As metacarpal nailing has been shown to be simple and fast, with unprecedented construct strength and low complications leading to a rapid return to function, it is increasingly becoming the standard of care.
The Field Orthopaedics NX Nail was selected as an ideal implant for this patient due to her age, concerns with loss of reduction and desire for an optimal cosmetic outcome. As the NX Nail has been designed with an anatomically inspired head and increased distal engagement, it was considered that this implant would provide increased stability, allow rapid return to function, and reduce the risk of deformity.
When comparing other intramedullary fixation options Dr Wurapa put his confidence in the NX Nail due to the increased implant engagement and control of the fragment. He also notes the significant progression of modern orthopaedics away from pins and plates, due to the inferior mechanical strength and insult to the soft tissues respectively.
Reduction
Intraoperatively the fractures were reduced, and the ideal implant diameter determined using the available template guides. A retrograde percutaneous guidewire was placed from the dorsal third of both metacarpal heads down the shaft. Ideal guidewire position was verified with fluoroscopic imaging and a 3mm incision made around each wire with a 15-blade scalpel.
Bone preparation
The depth gauge was used to determine implant length before the guidewire was advanced temporarily across the CMC joint to avoid inadvertent extraction with subsequent steps. The cannulated drill was passed over each guidewire under imaging for the proposed length of the nail.
Definitive fixation
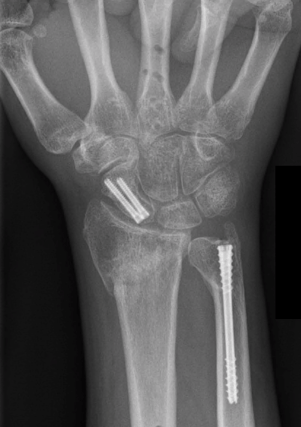
The NX Nail implants (lengths of 50mm for third metacarpal, and 45mm for fourth metacarpal) were then manually placed over each guidewire and seated into place under fluoroscopic imaging. Imaging showed excellent reduction and stabilisation had been achieved for both fractures.
Below: Intra-Operative Imaging


Closure
Following confirmation of definitive fixation, the guidewires were extracted, and the wounds closed with 5-0 prolene sutures. A soft dressing and hand-based splint which allowed for the interphalangeal joints to be free was placed for 3-5 days. This was followed by active mobilization as tolerated with a home exercise program and light daily activity. As the NX Nail has sufficient strength for immediate return to function and the technique has minimal insult to the soft tissue, formal therapy is rarely required. In this case the patient was able to return to normal duties as tolerated.
FOLLOW UP
The follow up period was uneventful, and the patient progressed well with a good outcome. On presenting for her final follow-up at six weeks there was full functional motion with no pain or restrictions.
DISCUSSION
In this case Dr Wurapa was able to effectively manage a commonly seen fracture in a patient that had concerns about the potential outcomes. In this treatment approach, it is noted that the significant control of the distal fragment and reliability of the implant allowed for immediate return to function.
This in turn addressed the substantial morbidity that was previously distressing the patient. The key benefits of the Nx Nail is the simplicity of use, along with reduced operating time which provides benefits to the surgical facility. Combined with the supra-physiological mechanical strength of the implant, and the minimally invasive surgical technique, this provided best-in-class
benefits for the patient; allowing them to rapidly return to their normal life and move on from their traumatic injury.
Dr Wurapa states that the NX Nail has become his go to option for the management of unstable extra-articular fractures of the hand. The extensive size offering from 2.0mm through to 5.0mm diameter provides options for both the metacarpal and phalangeal trauma. The non-compressive design maintains length and conforms to AO principles of fracture management. The increased bone engagement reduces the requirement for immobilisation which is thought to improve functional outcomes.
FO-003276-MM Version 1 Sep 2022 6